Personalized Obstetrics Services in Manchester, NH
OB Navigation Links
Obstetrical Services We Provide
- Preconception counseling
- Genetic testing
- Certified nuchal translucency ultrasound
- Level II screening ultrasound
- High-risk obstetrical care
- Access to nutritional counseling
- Diabetes screening and education
- Antenatal testing for high-risk pregnancies
- Non-Stress Test
- 3D ultrasound
- Immunizations
- Depression screening
- Postpartum depression support
- Lactation consultation
- Delivery at Elliot Hospital, by the doctors you meet in the office, with Level III NICU support
Appointment Schedule
-
Your first visit (8 weeks)
When you come to the office for your 8 week visit, we ask that you bring your medical history forms and other registration materials completed. We will review your medical history: obstetric, gynecologic, past medical/surgical, substance use and family histories. We will also review your medications and allergies along with any pertinent medical history from your partner.
Our nurses will offer counseling and advice on several issues pertaining to your pregnancy.
- How is your mood? Refer to your EPDS here.
- Substance use
- Genital herpes
- Vaccinations
- Travel
- Exercise and nutrition
- Environmental work hazards
- How to safely care for your pets
- Wear your seatbelt
- Car seat safety
- Circumcisions
- Childbirth education
- Postpartum feeding plans
- Pediatrician
During this visit there will be a series of prenatal labs that will test your blood type, blood count and screen for infections (syphilis, hepatitis B and C, HIV, rubella, gonorrhea and chlamydia). All of the results will be reviewed with you at your next appointment.
-
Your second visit (12 weeks)
At 11-13 weeks you will have a visit with one of our physicians. We will review your history and make an individualized plan for your prenatal care. You will have an exam at this visit. If you opt for genetic screening, you will also have an ultrasound and blood work.
-
Schedule of visits
For most women, visits will be every 4 weeks from 12-28 weeks, every 2 weeks from 28-36 weeks and then weekly until delivery. We will check your weight, blood pressure and fetal heartbeat at every visit. Beyond 20 weeks we will measure your baby's growth by the height of your uterus. If there are any complications, we will adjust your visit schedule accordingly.
-
Routine Screening
The Rh Factor - we will test for your blood type early in the pregnancy. Women with a negative blood type have the potential to form antibodies against fetal red blood cells, which can make the baby anemic. Rhogam is a medication that blocks this response and is given at 28 weeks, following any bleeding episodes during the pregnancy, and after delivery if the baby's blood type is Rh+.
Vaccinations - the Centers for Disease Control (CDC) recommends that women pregnant during the flu season receive the flu shot. Pregnant women are also recommended to get the Tdap vaccine at 27-36 weeks. Even if you have had it in the past 10 years you will make new antibodies that cross the placenta and protect your baby from whooping cough.
Anatomy ultrasound - this involves a complete survey of the baby between 19-20 weeks. This in-depth evaluation requires the full attention of our sonographer and we may recommend further images or discussion. We respectfully request your attention as well. Therefore photos, video recording or live chatting is prohibited with any ultrasounds.
Gestational diabetes and anemia - we will give you a sugary drink with instructions on how to drink it for your 26-28 week visit. We will draw blood at that visit to test for diabetes and signs of anemia. You do not need to fast for these tests.
Glucola Blood Test Instructions
Vaginal culture for group B strep - this swab of your vaginal area is performed at your 36 week appointment. Group B strep is a normal bacteria that is naturally found in the vagina and is not harmful to women or a developing fetus. However, it can be harmful to your infant if exposed at the time of delivery. If you test positive for this bacteria, you will receive antibiotics during labor and delivery.
Mood disorders - written questionnaires are used at intervals throughout the pregnancy and postpartum period to monitor for signs of depression or anxiety. Your emotional health is just as important as your physical health - if you have concerns about your mood at any visit, we encourage you to let us know. You don't have to wait until a designated screening visit.
Carrier Screening, Genetic Screening, Genetic Testing
Carrier screening looks for disorders that can be inherited from one or both parents and lead to significant physical impairment or shortened lifespan. A review of your family history helps decide what testing is recommended. These can include Cystic Fibrosis (CF), Spinal Muscular Atrophy (SMA), Fragile X and Tay Sachs.
- CF is a chronic respiratory disease. Caucasians are more commonly carriers of this class of genetic mutation, however, both parents have to pass on the gene for the disease to be present.
- SMA is a severe form of muscular dystrophy that leads to significant physical disability and shortened lifespan.
- Fragile X is most often expressed as varying levels of mental delay in boys and girls. Girls can be silent carriers or can experience gynecological issues later in life.
- Tay Sachs results from an error in metabolism that leads to physical, neurologic and developmental delays and, ultimately, early death.
- Additional testing may be offered based on your ethnicity or family history.
This testing is not mandatory.
Disclaimer: We no longer use Invitae for our carrier screening. However, this video is a great overview of what carrier screening is all about.
Genetic Screening
- We currently offer Non-Invasive Prenatal Sampling (NIPS) which screens for Down Syndrome (Trisomy 21), Edward's Syndrome (Trisomy 18) and Patau Syndrome (Trisomy 13). This testing can be done as early as 10-12 weeks and looks for fragments of the baby's genetic material in maternal blood. Since this test is performed on a maternal blood sample there is no risk to the pregnancy. If there is an abnormal result, options for additional testing will be discussed (see Genetic Diagnostic Testing).
- We also offer AFP (alpha-fetoprotein) screening at your 16 week visit. This is another maternal blood draw that looks for neural tube defects like spina bifida.
This testing is not mandatory.
Disclaimer: We no longer use Invitae for our NIPS testing. However, this video is a great overview of what NIPS is all about.
Diagnostic Genetic Testing offers the most complete look at the baby’s chromosomes. With this invasive form of testing, cells are taken either from the fetal parts of the placenta (chorionic villus sampling or CVS) or from the amniotic fluid surrounding the baby (amniocentesis) and all of the baby’s chromosomes are tested. The advantage is more complete testing with 99.9% accuracy. However, there is a small risk of miscarriage.
- CVS is performed in the first trimester (10-12 weeks). Risk of miscarriage is 1/100 (1%).
- Amniocentesis is performed in the second trimester (16 weeks). Risk of miscarriage is 1/300 (0.3%).
Click on the following link for Quest billing information:
Frequently Asked Questions
-
Q: How much weight should I gain?
A: Underweight women with a low weight gain during pregnancy appear to have an increased risk of having a low birth weight infant and preterm birth. On the other hand, obese women have an increased risk for having a large for gestational age infant, post-term birth, and other pregnancy complications.
- Underweight women (BMI <20): 30-40lbs
- Normal weight women (BMI 20-25): 25-35lbs
- Overweight women (BMI 26-29): 15-25lbs
- Obese women (BMI >29): up to 15lbs
-
Q: What comprises a healthy diet in pregnancy?
A: The first step toward healthy eating is to look at your daily diet. Having healthy snacks during the day is a good way to get the nutrients and extra calories that you need. Pregnant women need to eat an additional 100-300 calories per day, which is equivalent to a small snack such as half of a peanut butter and jelly sandwich and a glass of milk.
-
Q: What foods should I avoid during pregnancy?
A: You should avoid the following foods:
- Raw meat - Avoid uncooked seafood and undercooked beef or poultry due to risk of bacterial contamination, toxoplasmosis and salmonella.
- Deli meats - Avoid deli meats, or heat them until they steam, due to risks of listeria contamination.
- Fish with mercury - Avoid fish with high levels of mercury including shark, swordfish, king mackeral and tilefish. The FDA and EPA recommend 2-3 servings of seafood per week.
- Smoked seafood - Refrigerated, smoked seafood should be avoided due to risks of listeria contamination.
- Raw eggs - Raw eggs or any foods containing raw eggs can be contaminated with salmonella. This includes some homemade caesar dressings, mayonnaise, and homemade ice cream. Cook eggs thoroughly until the yolk is firm.
- Soft cheeses - Imported soft cheeses may contain listeria. Soft cheeses made with pasteurized milk are safe.
- Unpasteurized milk - May contain listeria which can lead to miscarriage.
- Pate - Refrigerated pate or meat spreads should be avoided due to risks of listeria.
- Caffeine - Limit caffeine intake to 200mg or less each day (this can be 1-2 cups of coffee a day depending on the size and strength of your coffee). Excess caffeine may be associated with miscarriage, preterm birth, low birth weight and withdrawal symptoms in infants.
- Unwashed vegetables - Wash all vegetables well to avoid exposure to toxoplasmosis which may contaminate the soil where vegetables are grown.
-
Q: What vitamins are recommended?
A: We recommend a prenatal vitamin that contains folic acid prior to conception, throughout pregnancy and postpartum while breastfeeding. We also recommend 2000 units of vitamin D3 daily and 200-300mg DHA (which may be included in your prenatal vitamin). Please check with your provider before taking any additional vitamins, herbs or other supplements as some may be unsafe in pregnancy.
-
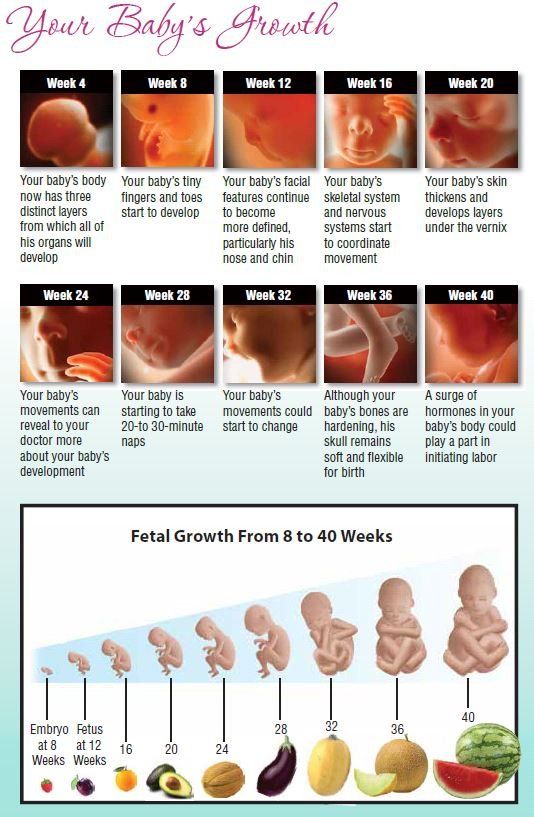
Q: When will I feel my baby move?
A: Sometime between 16-25 weeks of pregnancy, mothers will begin to feel fetal movement. Initially, movements will be infrequent and may feel like butterfly flutters. As your baby grows, you will feel movement more often. It is recommended to start counting fetal movements beginning at 32 weeks once daily until you get 10 movement within 2 hours. A good time to do this is 20-30 minutes after breakfast or dinner. If you are concerned about movement, eat or drink something with sugar, lie on your side and press your hands on your belly. If you continue to have concerns, contact the office.
-
Q: Are these symptoms normal?
A: Common symptoms of pregnancy
- Nausea/Vomiting - feeling nauseous during the first three months of pregnancy is very common. For some women, it can last longer, while others may not experience it at all. Try to eat 5-6 smaller meals a day in order to keep your stomach full at all times. Try bland foods like plain crackers, toast, dry breakfast cereal as well as carbonated drinks like gingerale or 7-Up. Ginger is a natural treatment for nausea. Peppermint can also be used. Some over-the-counter medications are also safe (see below). If the symptoms become severe, or you are unable to keep fluids down without vomiting for more than 12 hours, contact the office.
- Discharge - an increase in vaginal discharge that is white and milky is common in pregnancy. If the discharge is watery or has a foul odor, call the office.
- Spotting - light bleeding can be common, especially in the first 12 weeks of pregnancy. It may occur after intercourse, cervical exams, vaginal ultrasounds or strenuous activity or exercise. If the bleeding is heavy or accompanied by pain, contact us immediately.
- Constipation - is a common complaint which can be related to hormone changes, low fluid intake, increased iron or lack of fiber in your diet. Try to include whole grains, fresh fruit, vegetables and plenty of water. There are also safe over-the-counter medications. If you develop hemorrhoids, try sitz baths three to four times per day for 10-15 minutes each time. If the pain persists, contact the office.
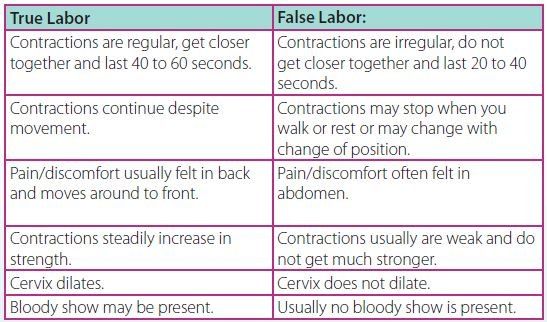
- Cramping - experiencing some cramps and contractions are normal. When they occur, empty your bladder, drink 1-2 glasses of water and try to rest. If you are less than 37 weeks pregnant and having more than six contractions in an hour, after trying these measures, contact the office.
- Leg cramps - cramping in your legs or feet can also be common. Eating bananas, drinking more lowfat/nonfat milk and consuming more calcium-rich foods like dark green vegetables, nuts, grains and beans may help. To relieve the cramp, try to stretch your leg with your foot flexed toward your body. A warm, moist towel or heat pad wrapped on the muscle may also help.
- Dizziness - you may feel lightheaded or dizzy at any time during your pregnancy. Try lying down on your left side and drink 1-2 glasses of water. If symptoms persist, contact the office.
- Swelling - because of the increased production of blood and body fluids, normal swelling, also called edema, can be experienced in the hands, face, legs, ankles and feet. Elevate your feet, wear comfortable shoes, drink plenty of fluids and limit sodium. Supportive stockings can also help. If the swelling comes on rapidly, or is accompanied by headache or visual changes, contact us immediately.
- Heartburn - you may experience heartburn throughout the pregnancy, especially during the latter part of your pregnancy when your baby is larger. Try to eat 5-6 smaller meals a day and avoid laying down immediately after eating. Some over-the-counter medications are also safe for use (see below).
- Aches and pains - as your baby grows, backaches are common. You may also feel stretching and pulling pains in the abdomen or pelvic area. These are due to pressure from your baby's head, weight increase and the normal loosening of joints. Practice good posture and try to rest with your feet elevated. You may also treat with heat and Tylenol.
-
Q: Which medications are safe in pregnancy?
A: During pregnancy, women can be more susceptible to ailments like cold and flu and other conditions. Only certain medications are safe during pregnancy. Please click the link for a list of safe medications. Follow the labels for dosage and directions. Contact the office with questions.
-
Q: When should I be evaluated?
A: If you experience any of the following, please call our office immediately. If our office is closed, stay on the line and you will be connected to the answering service.
- Continuous leaking of fluid (water broken)
- Abdominal trauma or car accident
- Heavy bleeding
- Fever greater than 101 degrees
- Decreased fetal movement
- Urinary tract infection
- Headache with visual changes
- Painful contractions greater than 6 times an hour if less than 37 weeks
-
Q: Why am I so tired? What is the best sleep position?
A: It's normal to feel more tired. You may also notice you need more sleep than usual. Try to get at least 8-10 hours per night. Listen to your body.
Try to sleep on your side to allow for maximum blood flow to the baby. Lying on your back can cause your blood pressure to drop. You may also find it helpful to put a pillow behind your back and between your knees to improve comfort. As your pregnancy progresses, use more pillows and frequent position changes to stay comfortable.
-
Q: Can I use a Jacuzzi?
A: Using a Jacuzzi or whirlpool bath is not recommended during the first trimester and should be limited to 15 minutes or less in the second and third trimester with the water temperature not exceeding 100 degrees.
-
Q: Can I travel?
A: Traveling is safe during uncomplicated pregnancies. After 36 weeks, we recommend staying close to home. When you do travel, be sure to take breaks to stand up/walk around at least every 2 hours. If traveling by vehicle, wear a seat belt, positioning it under your abdomen as your baby grows. If you are involved in a car accident, please call the office immediately. If you are traveling beyond 24 weeks, we may recommend you bring a copy of your medical records with you. There are also travel restrictions due to increased risks of some infections during pregnancy. These restrictions are updated regularly by the Center for Disease Control (CDC) and posted on their website. Please let us know about any upcoming travel.
-
Q: Can I care for my pets?
A: If you have cats, please let us know. Avoid changing the litter box or use gloves to change it. Toxoplasmosis is a rare infection that you can get from cat feces.
-
Q: What do I need to know about dental care?
A: Your teeth and gums may experience sensitivity throughout the pregnancy. Inform the dentist of your pregnancy and shield your abdomen if x-rays are necessary. Contact our office with any questions.
-
Q: Can I go to the salon for treatments?
A: Hair coloring and nail care should always be done in large, well-ventilated areas. If possible, avoid treatments in the first trimester.
-
Q: Can I exercise?
A: 30 minutes of exercise is recommended daily in uncomplicated pregnancies. This may include walking, jogging, biking, aerobics, yoga, swimming, etc. Weight training is acceptable. Listen to your body during exercise and drink plenty of fluids. After 20 weeks, avoid lying flat on your back and avoid activities with a high risk of falling or trauma to your belly (i.e. skiing, kickboxing, horseback riding).
-
Q: Can I have sex?
A: You can have sex unless you are having complications or sex becomes too uncomfortable. If you are having any of the following conditions, sex and exercise should be avoided - vaginal bleeding, leaking amniotic fluid, preterm labor, chest pain, regular uterine contractions, decreased fetal movement, growth restricted baby, headache, dizziness or general weakness.
Preparing for Labor and Delivery

Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
-
Pre-register with the hospital
We are affiliated with:
Elliot Hospital
1 Elliot Way
Manchester, NH 03103
Please call the hospital at 663-5663 to pre-register for Labor & Delivery. Registering before you are in labor will make your admission process smoother.
-
Attend educational courses
There are educational courses on labor and delivery, breastfeeding, infant CPR and baby care available. Consider these classes especially if you are a first time parent! The Elliot Hospital offers a variety of courses. Ask your providers about other resources in the area.
-
Take a Virtual Tour of Labor & Delivery
Click here.
-
Consider pain management options
If desired, there are several options to provide pain relief while you are in labor. We are supportive of whatever you choose.
- Nitrous oxide - this is an inhaled gas that dissociates or "separates" you from the contractions. It is patient-controlled, acts and resolves quickly and does not cross the placenta.
- Nubain - this narcotic is given through injection or IV and helps take the edge off strong contractions. It can make you sleepy, so we avoid giving this near delivery.
- Epidural - this safe and popular option is administered by an anesthetist and requires a fine, thin catheter or tube to be placed in your back during active labor. Medicine slowly drips through the tubing to provide pain relief throughout labor. It is removed after delivery.
- Local - many patients deliver without pain medication. Sometimes we need to give a small injection of numbing medicine, called lidocaine, for stitches. It feels like a small pinprick.
-
Choose a doctor for your baby
You will need to decide on a doctor for your baby by the time you deliver. The hospital will send your baby's information and test results to your chosen doctor. Your baby is commonly seen within 1 week after birth. You will need to contact the doctor's office prior to delivery and make sure they are accepting your insurance and are taking new patients. We can provide you with a list of doctors if you have trouble locating one.
-
Obtain and install a car seat
You must have a car seat installed in your vehicle before taking your baby home. By law, children must be in a federally approved, properly installed, crash-tested car seat for every trip in the car beginning with the trip home from the hospital.
-
Research cord blood banking
Your baby's blood is a valuable source of cells that could be used by your baby or another family member to treat some life-threatening diseases. It can easily and safely obtained immediately after delivery. Parents can choose to have their baby's blood saved; however the decision must be made before birth. Insurance does not generally cover this. If interested, you can order a kit and bring it with you to delivery. Ask your provider for information.
-
Learn more about breastfeeding
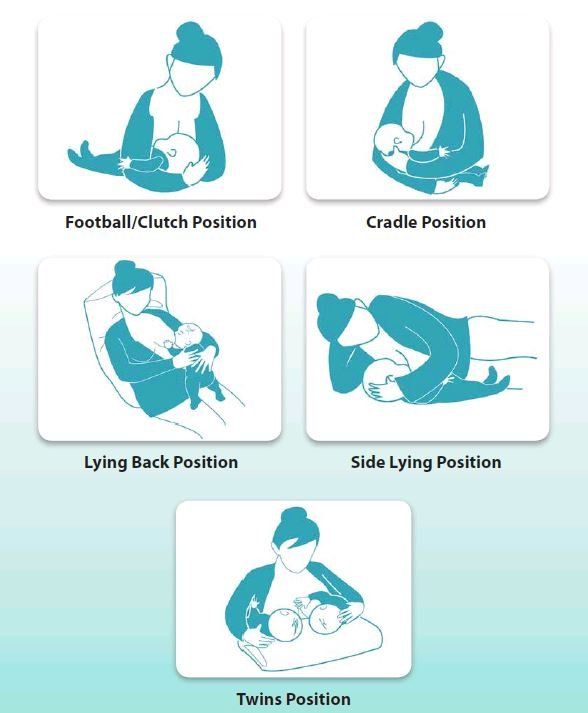
Human milk is perfectly designed nutrition for babies. Babies who are breastfed get fewer infections and are hospitalized less. Mothers that breastfeed burn 500 calories a day which can help lose extra weight. Breastfeeding can also reduce a woman's risk of developing breast cancer. After delivery, the nurses and lactation specialists are there to help you learn the art of breastfeeding. Learn more about breastfeeding here.
-
Consider circumcision
A circumcision is the removal of excess foreskin from the penis. We can perform this optional procedure for your baby in the hospital. It may help reduce infections and cancer of the penis. Please let your provider know if you would like this performed. We respect your choice if you decide not to proceed with circumcision.
Labor and Delivery
-
Induction
Your due date is considered 40 weeks. We recommend additional testing for your baby at 40-41 weeks. We induce labor at 41+ weeks, or sooner if there are concerns. Induction is a process where we give medication to stimulate contractions. It can take more than 24 hours to work and can increase the chance of cesarean delivery, especially if your cervix has not started to thin or dilate on its own. Elective induction is not considered prior to 39 weeks to allow the baby time to fully grow and develop.
-
Cesarean birth and recovery
A cesarean birth may be planned or unplanned. Nurses, anesthesia staff and your physician will be with you in the operating room. If necessary, a group of neonatal health care providers will also be with you. Your blood pressure and heart rate/rhythm will be monitored, and a nurse will listen to your baby's heart rate before the procedure. Your baby is usually delivered in a short period of time once surgery begins. Once delivered, it will take approximately 45-60 minutse to complete surgery. Your incision will be closed with staples or sutures. You will then be moved to the recovery room.
-
Initial recovery after cesarean birth
The immediate recovery period is similar to the recovery period of a vaginal birth. Rest to conserve your strength. You, your baby and your support partner will remain in the Labor & Delivery recovery room for approximately 2 hours. During this time you and your baby will be monitored closely.
-
Episiotomy/forceps/vacuum
We plan to help you deliver your baby with the least amount of trauma. We will recommend using forceps or a vacuum only if medically indicated. Episiotomies are not routinely needed and many women deliver without the need for any stitches. Sometimes we need to make a small incision at the vaginal opening to help deliver. We make sure you are numb if you don't have an epidural, and will stitch the area after delivery. The stitches dissolve over time and do not need to be removed. We provide you with medicine to keep you comfortable after delivery.
We are highly skilled in techniques for operative delivery. We will recommend them only if medically indicated. Our goal is to deliver your baby in the safest manner. There are definitely times when this is the safest way to help your baby into this world.
Breastfeeding
-
Full-time Nursing
- Full-time nursing means you can nurse the baby during the workday OR you want to be able to express milk often enough (at least every 3-4 hours) to be able to provide all the milk your baby needs when separated from you. Formula will only be used in rare instances when you don't have quite enough breast milk.
- Occasional bottle feeding should begin about 4-6 weeks after delivery, even if you are not planning on returning to work, until your baby is 7 months old. Introduce the baby to the bottle 1-3 times per week by letting Dad or someone else feed some of your expressed milk. It doesn't need to be a "full" feeding; the intent is for the baby to get used to drinking milk from a rubber nipple and bottle.
- About 7-14 days prior to returning to work, you will need to start expressing milk by hand or with a pump so that you have enough for your first day back at work. Most women find they have more success expressing milk in the morning. Try this about 1 hour after the baby nurses. Just express for 10-15 minutes at the most and do it consistently each day. Expressing more than 1-2 times per day is not recommended. Don't worry if you only get a small amount when you begin.
- Milk can be stored in baby bottles, a pitcher, or any clean container in the refrigerator. Milk can be kept in the refrigerator for 5 days. After 5 days it should be frozen or discarded.
- Breast milk, when removed from the refrigerator or freezer, may appear discolored (yellow tinged, bluish green, even a little brown). This does not mean the milk is bad. Always check breast milk to be certain it does not smell or taste bad. Because breast milk does not look like cow's milk when stored, taste and smell, not color, should determine if the milk is good.
- When you are at work express milk every 2-4 hours. You do not have to express at the same time every day but express milk often enough to prevent engorgement. What you express each day is what is used the next day.
- You should nurse as soon as you can when you get home and as exclusively as you can. If you find that your milk supply has dropped, try expressing milk before bedtime to help stimulate the supply a little.
-
Part-time Nursing
- Part-time nursing involves the ability to nurse the baby or express milk occasionally during the workday. You do not expect to be able to feed or express milk often enough to maintain a full milk supply and meet all of your baby's needs with your breast milk. Formula will be used frequently to provide all or most of the milk your baby needs while you are at work.
- This option works better when babies are older and mothers do not have long workdays and long commutes. Mothers with babies less than 3-4 months old risk losing more of their milk supply than they planned on if they are not able to express milk at all during the day. "Comfort expressing" (removing just enough milk to avoid discomfort from overly full breasts) can help you meet this goal better. Another variation of this option is expressing milk (even on a limited basis) at work until the baby reaches 3-4 months of age. Then you can discontinue expressionm use formula while you are working, and continued frequent breastfeeding when you are home.
- About 7-14 days prior to returning to work eliminate one or two feedings that you will miss while you are at work. Replace breastfeeding at those two feedings with a bottle of formula or breast milk. If your breasts are uncomfortable place some ice on your chest or express just enough for comfort. This will reduce the amount of stimulation your breasts receive and thereby, decrease the milk supply a little.
- Try to express milk at work if you can, even if it is not every day or the same time every day. Nurse as much as you can when you are at home.
-
Football/Clutch Position
- Put a pillow or two at your side to help support your arm and your baby
- Support your baby's neck and the lower back of his head in your hand, with your forearm supporting his upper body against your side
- Support your breast with your hand in an "L" or "C" position, thumb on top of your breast, fingers below, away from your areola
- Tickle your baby's lip until he opens WIDE, and then quickly pull him onto your breast. Be patient. This may take a minute.
- Make sure your baby's lips are behind the nipple, encircling the areola
- The tip of your baby's nose should be touching the breast
-
Cradle Position
- Place a pillow or two in your lap to support your baby
- Place your baby's head in the crook of your arm
- Make sure your baby is turned toward you, chest to chest, at breast level
- Support your breast with your hand in an "L" or "C" position, thumb on top of your breast, fingers below, away from your areola
- Tickle your baby's lip until he opens WIDE, and then quickly pull him onto your breast. Be patient. This may take a minute.
- Make sure your baby's lips are behind the nipple, encircling the areola
- The tip of your baby's nose should be touching the breast
-
Side Lying Position
- Lie on your side with pillows supporting your back and your top leg, which is bent forward
- Place your baby on his side facing you
- Support your breast with your hand in an "L" or "C" position, thumb on top of your breast, fingers below, away from your areola
- Tickle your baby's lip until he opens WIDE, and then quickly pull him onto your breast. Be patient. This may take a minute.
- Make sure your baby's lips are behind the nipple, encircling the areola
- The tip of your baby's nose should be touching the breast
-
Helpful Hints
- Vary nursing positions for the first week.
- Breastfeed frequently, about every 1.5-3 hours. Keeping your baby on an artificially longer schedule may make him frantically hungry and increase the likelihood of vigorous nursing and tender nipples.
- Release the suction before you remove your baby from the breast. Do this by placing a clean finger in the side of your baby's mouth between his jaws. Don't take him away until you feel the suction break.
- After nursing your baby, express a little breast milk and massage it into your nipples and areola, then air dry. Leave them open to air as much as possible.
-
Sore Nipples
Breastfeeding is meant to be a comfortable, pleasant experience. However, many new mothers still find their nipples tender for the first few days when the baby starts nursing. This usually disappears in 1-2 weeks. Proper positioning and latch can help prevent tenderness. If your nipples do become sore, try these suggestions:
- Use deep breathing, soft music or other relaxation techniques before and during breastfeeding.
- Limit the nursing time on the sore nipple.
- Express a little milk first to stimulate let down.
- Massage your breasts while nursing. This helps stimulate the milk to flow.
- Use non-plastic lined bras and/or bra pads. change the pads frequently to keep the nipple dry.
- If your nipples become dry or cracked, use a little USP Modified Lanolin on them. This forms a moisture barrier so they stay dry.
-
Suggested Breastfeeding Books
- "The Womanly Art of Breastfeeding" by La Leche League International
- "Breastfeeding Your Baby" by Sheila Kitzinger
- "Bestfeeding: How to Breastfeed Your Baby" by Mary Renfrew, Chloe Fisher, Suzanne Arms
- "The Nursing Mother's Companion" by Kathleen Huggins
Postpartum Depression
| POSTPARTUM “BLUES” | DEPRESSION AND ANXIETY DURING PREGNANCY AND POSTPARTUM | POSTPARTUM PSYCHOSIS | |
|---|---|---|---|
| How common is it? | NORMAL. 50-80% of women experience the blues. | 15% - 23% of women, more often in teens. 10% of men. | 1-2 per 1000 women. More often if someone has a history of mental illness. |
| When does it start and how long does it last? | Can occur any time in the first week. Usually gone by 2-3 weeks after birth. | Can occur any time in pregnancy or the first year after birth. It can start gradually or suddenly. Unless treated, it may not go away. | Usually occurs within the first 4 weeks after birth. Needs treatment immediately. |
- Frequent crying
- Sleep disturbances (insomnia/excessive sleeping)
- Appetite disturbances (eating too much or too little)
- Anxiety/panic attacks
- Feelings of anger/irritability
- Over-concern or lack of concern for baby
- Scary thoughts or mental pictures
- Reliving past trauma
- Feelings of guilt and worthlessness
- Feeling overwhelmed/unable to cope
- Loss of interest in things you previously enjoyed
- Fear of harming baby or yourself
- Seeing or hearing things that others do not.
- Agitation, restlessness, irritability
- Mania: feeling speeded up, distracted, excitable, having a decreased need to sleep, or exhibiting fast, pressured speech
- Confusion
- Paranoia (extreme fears)
- Extreme mood swings
- Inability to reason, delusions
- Thoughts or plan of hurting yourself or baby
- Call us at 622-3162 to schedule an appointment. We have nurse practitioners who specialize in perinatal behavioral health and we are known for our compassionate care.
- Treatment may include counseling/therapy or medications that are safe during pregnancy and breastfeeding.
- We recommend good self-care including 4-5 consecutive hours of sleep, small, healthy, frequent meals, exercise, and limiting caffeine.
- There are also pregnancy/postpartum depression support groups so you can connect with other new moms experiencing similar issues.
- Manchester Mobile Crisis Response Team: 1-800-688-3544
- Concord Mobile Crisis Response Team: 1-844-743-5748
- Center for Life Management (emergency services for Derry): (603)434-1577, option 1
- New Hampshire Coalition Against Domestic and Sexual Violence: 1-866-644-3574
- Manchester YWCA Women's Crisis Line: (603)668-2299
- Suicide Prevention Hotline: 1-800-273-TALK (8255)
Contact Information
- 150 Tarrytown Rd Manchester, NH 03103
- 77 Gilcreast Rd, Suite 1000 Londonderry, NH 03053
- Mon - Thu
- -
- Friday
- -
- Sat - Sun
- Closed
- Morning appointments starting at 7:30am
- Lunch-time appointments
- Evening hours on Thursdays (last appointment at 7pm)
Contact Us
We will get back to you as soon as possible.
Please try again later.